May 25, 2006, Lincoln Hall, an Australian climber descends from Mount Everest after an amazing climb and a successful summiting. On his way down, at an altitude of 8600 meters, Hall collapsed. His team couldn’t carry him down the mountain and left him abandoned on the snow. Through the satellite phone, his wife received the message that her husband is no longer alive.
Twelve hours later, leader mountaineer Dan Mazur a team of climbers, are doing the way up to the summit. The team found Hall abandoned. Hall is exhausted, suffering from severe frostbites, with an open suit, at the edge of a sharp cliff. Hall turns to them and says: ‘I imagine you’re surprised to see me here’. The team decides to do everything in order to save Hall, carrying him down the mountain and he was saved.
This is an extreme case with a good and a very surprising end to a much more common phenomenon called altitude sickness.

Altitude Sickness is a phenomenon that occurs when our bodies are in continuous conditions of oxygen deficiency, at heights of 2500 meters or more.
At first, symptoms are relatively mild, weakness, dizziness, lack of appetite. Then, one will develop more severe symptoms of muscle fatigue, kidney pain and, blurring. In severe cases of altitude sickness, more extreme symptoms of brain and lungs edemas might show up, leading to an immediate risk of life.
The body tries to adapt itself to the thinning air which is lack of oxygen. The body produces more red blood cells and produces an enzyme to release more oxygen from the hemoglobin to the body’s tissues. Intraoral pressure rises and pushes the air into lungs areas that are not normally used. The metabolic processes are accelerated. The energy stores are depleted and the body is unable to compensate for the lack of oxygen. Hence, symptoms begin to appear.
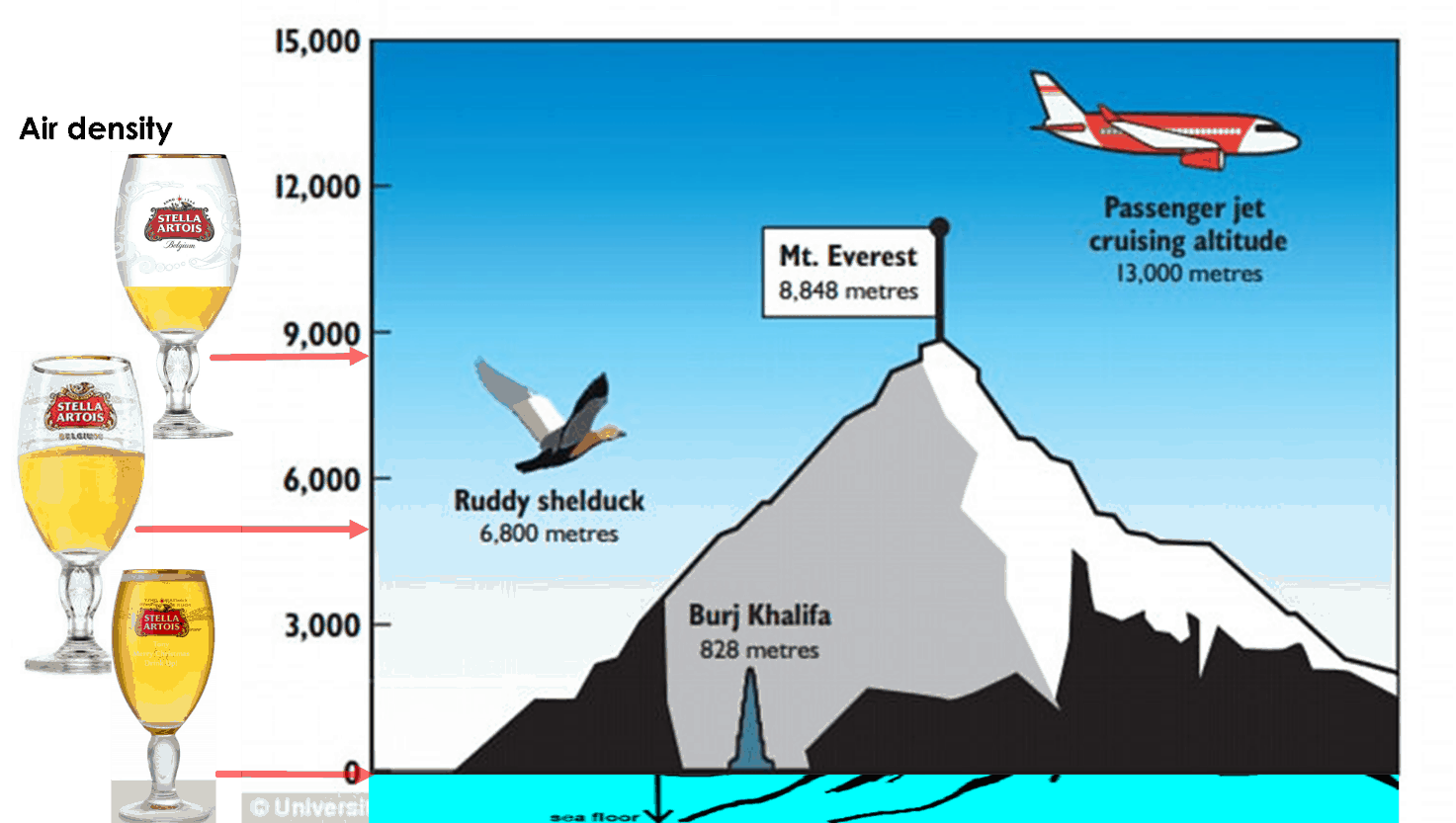
As an illustration, the air density at 5000 meters above sea level is about half the air density at sea level. On top of Mount Everest, the density of air is only one-third as compared to sea level.
We can define three categories of altitude sickness:
AMS-Acute Mountain Sickness – The common altitude sickness phenomenon usually affects travelers.
HAPE-High Altitude Pulmonary Edema- Lung edema develops at high altitudes.
HACE-High Altitude Cerebral Edema – Brain edema which may occur at high altitude as happened to the climber Lincoln Hall.
Blood actually flows out from the brain and inner skull pressure rises. This will cause confusion, blurring, loss of eye vision, orientation and will lead to death.
The Death Zone is the nickname among mountain climbers where there is not enough oxygen in the air. too low to be able to adapt to. normally considered at altitudes of 8,000 meters above sea level and beyond. It means that in such altitudes, the longer we stay the risk of death gets much higher.
Only very experienced individual climbers climbed up and returned from Everest summit without using supplemental oxygen.
In Nepal alone, helicopters rescue about 15 tourists a day, most of them due to altitude sickness.
The Kilimanjaro in Africa is a mountain that all you need to do for reaching its top is to trek. The mountain takes the lives 10 trekkers each year. Mostly because of altitude sickness.
The Aconcagua, the highest mountain outside the Himalayan ridge, takes the lives of 7~10 climbers each year, because of altitude sickness.
You don’t need to climb high mountains to suffer from altitude sickness as it might impact your body even at moderate heights of 2500 meters and above.
Although we all love to travel and like to see the worlds from a high vantage point, most of us don’t take into considerations the impact of high altitude.
So how can we overcome altitude sickness and continue to enjoy our trip or climb? Actually, let’s begin with what doesn’t help.
This info might surprise some of us but physical fitness is not a measure of our ability to acclimatize to lack of oxygen. Physical fitness indeed will help during the climb, but it is not an indication of lack of oxygen adaptation. Another thing we can notice is that the body can not completely acclimatize to optimum as we are able to maintain at sea level.
So what are the factors that can help us?
Carefully consider height acclimatization. At home-country or in the country of destination. We can point as examples, Lhasa, the capital of Tibet, and La-Paz in Bolivia. The altitude of these cities is more than 3,600 meters. Stay few days in these cities or lower points for acclimatization.
Plan your trip so that you can have night sleep at a lower point from today’s peak. This way you will encourage the body to produce more red blood cells in rest conditions.
When trekking above 2500 meters, plan to allow not a steep climbing up. Up to 500 meters accumulated height per day.
Every 800-900 meters allow a rest day to acclimatize. During rest days make easy day hikes to a higher point without high effort. Return for a night stay at the same original point or other equivalent height.
During more complex treks or climbs, we should have extra safety measures and it is advisable to carry with us blood’s oxygen saturation meter. This will allow us to confirm proper acclimatization to the lack of oxygen and a safer climb up.

If you suffer from dizziness, fatigue or lack of appetite, these are warning signs and always assume that the cause is altitude sickness – the body needs more rest and acclimatization before continuing to gain height. If possible it is also better to perform some descend to a safer acclimatization point.
We can prevent high altitude sickness by taking the proper drug-treatment.
Acetazolamide is the active ingredient in drugs like Diamox which prevents altitude sickness (among other usages).
Several studies have also shown that extracts from the Ginkgo Biloba tree leaves may also improve the ability to adapt to heights.
What’s more, we will drink more water – due to lack of oxygen the body works harder and needs fluids beyond the effort of the trek.
Avoid excessive drinking of alcohol, which slows breathing hence slows oxygen absorbance.
For those who embark for a climbing expedition and want a shortcut, stay in the hypoxic tent or use a hypoxic mask. These were designed to allow more acclimatization from home by sleeping in thin air conditions. Such training can shorten the climbing time of ordinary climbers on Everest to almost half the time.

Despite the prevention, how can we still take care of ourselves if we suffer from altitude sickness?
Descend! Go down in altitude! And rest, measure pulse and oxygen level if possible…. do not continue climbing until you get better acclimatization and maintain normal measures relative to the given conditions.
Taking acetazolamide at a higher dose is sometimes not too late and can also help with treatment.
Drug therapy with Dexamethasone or Nifedipine, which can respond to the more serious conditions of HAPE or HACE (lungs or brain edemas). Although often not part of the average traveler’s toolbox, these are important drugs for a climber to consider.
Taking oxygen supplement – even in regular treks, there are guides who, as part of the service, carry an emergency oxygen tank- you should check this before the trek or climb.
If your condition has deteriorated to life-threatening, and cannot be evacuated from the mountains, some of the base camps may have a pressure chamber that simulates air at sea level.

The information given in this article should not be treated as a medical recommendation. The writing concentrates knowledge gained from experience in hiking and mountain climbing and summarizes medical or technical articles on the subject but does not replace medical advice and personal acquaintance.

[…] Make sure your body adapts well to the lack of oxygen for your travel safety. Refer to the altitude sickness article for further data regarding altitude sickness and […]
[…] Acute Mountain Sickness from the lack of oxygen can lead to the progression to its severe manifestations: high–altitude pulmonary edema (HAPE) and high-altitude cerebral edema (HACE). […]
[…] Altitude Sickness-info, treatment and prevention […]
I am about to finish “Dead Lucky”, Lincoln Hall’s book about his climb and rescue. I can’t remember if he had the chance to use Diamox, or never a consideration. Hydration might have been a huge problem in his HACE. I am a very late arrival here, so I don’t expect a response.